Vitamin D's Renewed Promise in the Fight Against Cancer
Adequate vitamin D is linked to reduced cancer incidence and more effective treatment
Emerging research in the last several years is solidifying the role of vitamin D in cancer prevention and treatment, with numerous studies revealing its ability to hinder cancer cell growth, enhance immune function, and even improve the efficacy of conventional cancer therapies. This growing body of evidence is prompting a fresh look at the potential of this essential nutrient as a key player in oncology.
Once primarily recognized for its role in bone health, vitamin D is now understood to be a potent modulator of cellular processes that are critical in the development and progression of cancer. While not a standalone cure, recent findings underscore its significance as a complementary strategy in cancer management.
Unraveling the Mechanisms: How Vitamin D Combats Cancer
The anti-cancer properties of vitamin D are multifaceted and profound. At its core, the active form of vitamin D, calcitriol, interacts with the vitamin D receptor (VDR) present in cells throughout the body, including cancerous ones. This interaction triggers a cascade of molecular events that can effectively put the brakes on cancer.
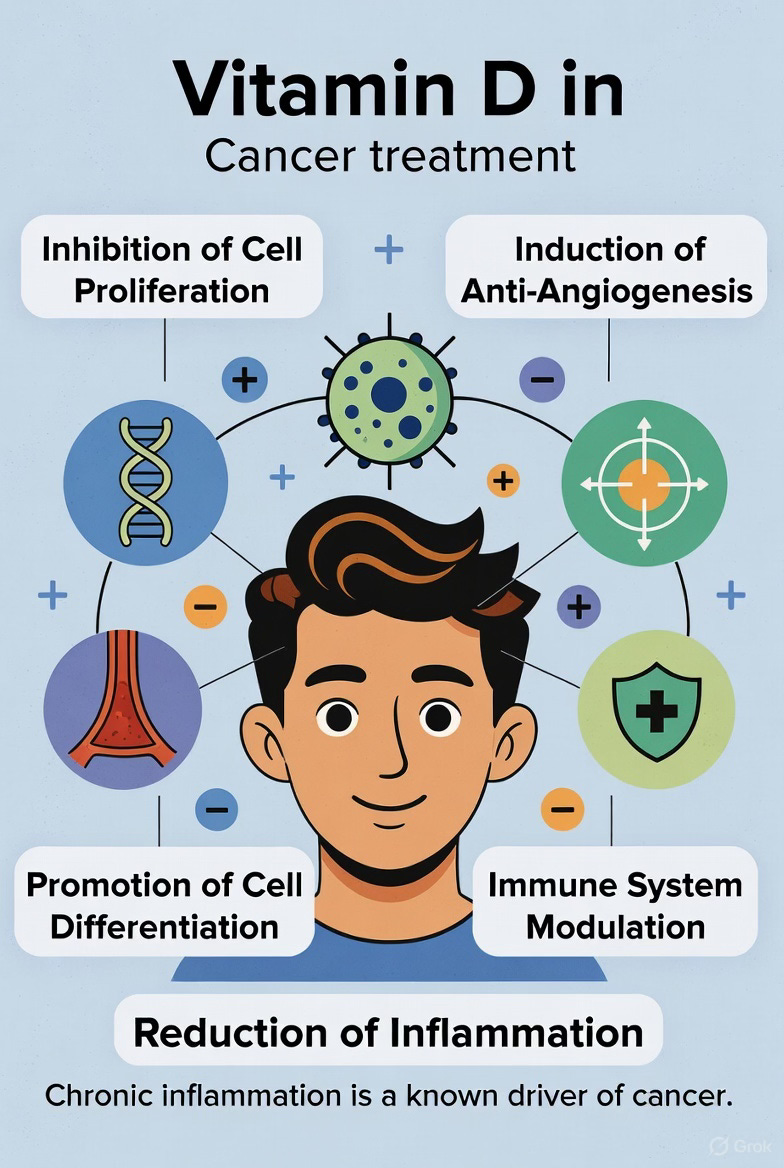
Key mechanisms of vitamin D’s anti-cancer action include:
Inhibition of Cell Proliferation: Vitamin D can arrest the uncontrolled growth of cancer cells by interfering with the cell cycle, the tightly regulated process of cell division (Bilezikian et al., 2019). It can halt cells in the G0/G1 or G2/M phase, preventing them from replicating.
Induction of Apoptosis: It promotes programmed cell death, or apoptosis, essentially telling cancer cells to self-destruct (National Cancer Institute, 2023).
Anti-Angiogenesis: Vitamin D can inhibit the formation of new blood vessels that tumors need to grow and spread, a process known as angiogenesis (Feldman et al., 2014). This effectively starves the tumor of vital nutrients.
Promotion of Cell Differentiation: It encourages cancer cells to mature and differentiate into more normal, less aggressive cell types (NCI, 2023).
Immune System Modulation: Emerging research highlights vitamin D’s ability to enhance the body’s natural anti-cancer immunity. It can modulate the activity of immune cells, such as T-cells, to better recognize and attack cancer cells (Fekete et al., 2025).
Reduction of Inflammation: Chronic inflammation is a known driver of cancer. Vitamin D has anti-inflammatory properties that can help quell this pro-cancerous environment (Reichrath & Reichrath, 2023).
Spotlight on Specific Cancers and Vitamin D
While research is ongoing across a spectrum of malignancies, several types of cancer have shown particularly promising connections to vitamin D status.
Colorectal Cancer: A substantial body of evidence points to a strong link between higher vitamin D levels and a reduced risk of colorectal cancer (Fekete et al., 2025). Some studies suggest that adequate vitamin D levels could cut the chances of developing this cancer by a significant margin (The Times of India, 2025). Furthermore, for those diagnosed with colorectal cancer, higher vitamin D levels have been associated with improved survival rates (Fekete et al., 2025).
Breast Cancer: Research suggests that maintaining sufficient vitamin D levels may be associated with a lower risk of developing breast cancer and could be linked to less aggressive tumors (Feldman et al., 2014; National Cancer Institute, 2016). One study found that low vitamin D was associated with tumor progression and metastasis in breast cancer (NCI, 2016). Excitingly, a recent Brazilian study demonstrated that low-dose vitamin D supplementation (2000 IU/day) nearly doubled the treatment response rate in women undergoing chemotherapy for breast cancer (São Paulo Research Foundation - FAPESP, 2025; Omodei et al., 2025). Again, imagine the magnitude of the response if physiological relevant doses (5000-8000 IU/day) of vitamin D were used.
Prostate Cancer: The relationship between vitamin D and prostate cancer is complex, but some studies suggest that adequate vitamin D levels could reduce the risk or severity of the disease (Medical News Today, 2021). Vitamin D deficiency has been linked to more aggressive forms of prostate cancer, particularly in African American men, highlighting its potential role in health disparities (Cedars-Sinai, 2023). Mechanistically, inflammation is thought to be a key link, with vitamin D potentially mitigating this cancer-promoting factor (U.S. Pharmacist, 2014).
Lung Cancer, Vitamin D and Keytruda
Perhaps the most significant cancer traditional treatment advance in the 21st century is the emergence of drugs that facilitate immune system attack on cancers. These drugs are known as immune checkpoint inhibitors (ICI), examples include Nivolumab (Opdivo), Pembrolizumab (Keytruda), Cemiplimab (Libtayo), and Dostarlimab (Jemperli). Their mechanism is to remove built-in safeguards in the immune system to prevent the immune system from attacking healthy tissue.
What could go wrong, right?
Anytime the topic is immune system, attention should turn to how is vitamin D involved.
Consistent with all of the above, patients with higher vitamin D levels have been shown to have better responses to ICI therapy (Bersanelli, et al., 2023). Some emerging clinical trial data suggest systematic vitamin D repletion during immunotherapy enhances efficacy and immune activation while maintaining safety (You, et al., 2025).
In a very exciting finding doctors in China have found that vitamin D acts synergistically with immune checkpoint inhibitor drugs to enhance the efficacy of those drugs in treating lung cancer (Zhang, et al., 2025) and melanoma (Galus, et al., 2023). Specifically, the findings were that patients with higher serum vitamin D levels had better responses and outcomes to the ICI cancer treatments.
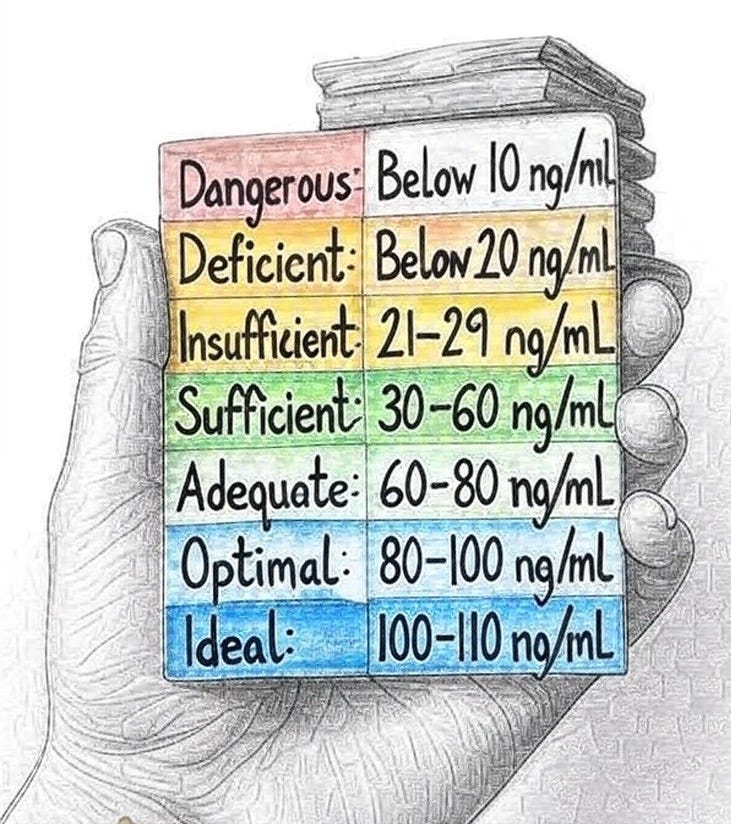
These studies define adequate or sufficient vitamin D levels as being around 30 ng/mL. While this appears to be a threshold level for these observed effects, imagine the results if vitamin D levels were in the optimal ranges of 80-100 ng/mL. It is important to appreciate that most of these studies on cancer and vitamin D use bottom of the barrel amounts of vitamin D because of the false information promulgated by the Institute of Medicine regarding US RDA of 600 IU/day. As a reference to how out of bounds the US RDA is recall that 40 year old skin exposed to summer sunshine for 15 minutes will make over 10,000 IU vitamin D.
Magnesium, Vitamin D and Colon Cancer: Local vs. Systemic Effects
In an intriguing insight into how little we really know about vitamin D and health, a 2025 study found magnesium supplementation increases gut bacteria that subsequently synthesize vitamin D. That vitamin D inhibits colorectal cancer development (polyps), particularly in females, suggesting complex nutrient-microbiome interactions in cancer prevention.
The study from Vanderbilt University Medical Center was a double-blind, precision-based randomized placebo-controlled trial investigating how magnesium supplements affect gut microbiome, vitamin D synthesis, and colorectal cancer risk. Key findings were:
Magnesium supplementation increased gut bacteria capable of synthesizing vitamin D locally in the gut, specifically Carnobacterium maltaromaticum and Faecalibacterium prausnitzii, which act to inhibit colorectal cancer carcinogenesis.
The effects were primarily seen in females, likely due to estrogen’s role in shifting magnesium from blood circulation into cellular uptake.
This suggests magnesium may reduce colorectal cancer risk through gut vitamin D synthesis that works locally rather than increasing systemic vitamin D levels.
Overall, the study provides new insights into how nutrition, the gut microbiome, and genetics interact to influence colorectal carcinogenesis and establishes a novel precision-based prevention foundation combining magnesium supplementation and microbiome modulation. It also highlights a hidden complexity in understanding vitamin D and cancer in that, simply knowing circulating levels of vitamin D may not be enough to appreciate the full impact of how vitamin D helps prevent cancer.
Takeaway: Magnesium enhances specific gut bacteria that then increase local vitamin D production which inhibits the development of polyps.
The Outlook and Recommendations
While observational studies consistently show a link between higher vitamin D levels and better cancer outcomes, results from randomized controlled trials on the preventive effects of supplementation have been more mixed (National Cancer Institute, 2023). These mixed results are due to using too low a dose of vitamin D.
Maintaining adequate vitamin D levels through a combination of sensible sun exposure, a balanced diet, and, when necessary, supplementation is a prudent strategy for overall health and may contribute to a reduced risk of cancer and improved outcomes for those diagnosed. As research continues to evolve, the “sunshine vitamin” is poised to play an increasingly important and well-defined role in the comprehensive approach to cancer prevention and care.
Reference List
Bersanelli, M., Cortellini, A., Leonetti, A., et al. (2023). Systematic vitamin D supplementation is associated with improved outcomes and reduced thyroid adverse events in patients with cancer treated with immune checkpoint inhibitors: results from the prospective PROVIDENCE study. Cancer Immunology, Immunotherapy : CII, 72(11), 3707–3716. doi.org/10.1007/s00262-023-03522-3
Bilezikian, J. P., Bouillon, R., & T’Sjoen, G. (Eds.). (2019). Vitamin D: Physiology, molecular biology, and clinical applications. Academic Press.
Cedars-Sinai. (2023, April 18). Study: Vitamin D may play a role in prostate cancer disparities.
Fekete, M., Lehoczki, A., Szappanos, A., & Priefer, R. (2025). Vitamin D and colorectal cancer prevention: Immunological mechanisms, inflammatory pathways, and nutritional implications. Nutrients, 17(8), 1351.
Feldman, D., Krishnan, A. V., Swami, S., Giovannucci, E., & Feldman, B. J. (2014). The role of vitamin D in the prevention and treatment of cancer. The Journal of Clinical Endocrinology & Metabolism, 99(6), 1953–1963.
Galus, Ł., Michalak, M., Lorenz, M. et al (2023).Vitamin D Supplementation Increases Objective Response Rate and Prolongs Progression-Free Time in Patients with Advanced Melanoma Undergoing Anti–PD-1 Therapy. Cancer, 129, 2047–2055.
Medical News Today. (2021, November 30). Vitamin D and prostate cancer: Benefits and more.
National Cancer Institute. (2016, April 14). Low vitamin D linked to breast cancer metastasis.
National Cancer Institute. (2023, May 9). Vitamin D and cancer.
Omodei, M. S., Chimicoviaki, J., Buttros, D. A. B., Almeida-Filho, B. S., Carvalho-Pessoa, C. P., Carvalho-Pessoa, E., & Nahas, E. A. P. (2025). Vitamin D supplementation improves pathological complete response in breast cancer patients undergoing neoadjuvant chemotherapy: A randomized clinical trial. Nutrition and Cancer, 77(6), 648–657.
Reichrath, J., & Reichrath, S. (2023). Vitamin D and cancer. In Vitamin D (pp. 1157-1181). Academic Press.
São Paulo Research Foundation - FAPESP. (2025, June 12). Vitamin D increases the likelihood that breast cancer will disappear with chemotherapy. EurekAlert!
Sun, E., et al. (2025). Magnesium treatment increases gut microbiome synthesizing vitamin D and inhibiting colorectal cancer: results from a double-blind precision-based randomized placebo-controlled trial. The American Journal of Clinical Nutrition, 122 (5), 1185 - 1194.
The Times of India. (2025, August 22). Vitamin D and colorectal cancer: New research shows how one can cut chances of having this cancer by almost 60%.
U.S. Pharmacist. (2014, November 17). Missing link between vitamin D and prostate cancer.
You, W., Liu, X., Tang, H. et al., (2025). Vitamin D Status Is Associated With Immune Checkpoint Inhibitor Efficacy and Immune-related Adverse Event Severity in Lung Cancer Patients: A Prospective Cohort Study. Journal of Immunotherapy, 46 (6), 236-243. doi.org/ 10.1097/CJI.0000000000000469
Zhang, Y., Xu, Y., Zhong, W., Zhao, J., Liu, X., Gao, X., Chen, M., & Wang, M. (2025). Vitamin D and Immune Checkpoint Inhibitors in Lung Cancer: A Synergistic Approach to Enhancing Treatment Efficacy. International Journal of Molecular Sciences, 26(10), 4511. doi.org/10.3390/ijms26104511
Included in all posts
General Recommendations for Vitamin D for Healthy Adults
The U.S. Institute of Medicine (IOM), now the National Academy of Medicine, recommends a dietary reference intake of 600 IU (International Units) per day for adults up to age 70, and 800 IU for those over 70, to maintain bone health (Institute of Medicine, 2011). However, this amount is orders of magnitude too low considering that the human body “uses” at least 4000 IU vitamin D per day.
However, there is a vast literature on the extraskeletal functions of vitamin D for maintaining optimal functioning of the immune system, muscular system and ideal aging that indicates that optimal levels of serum vitamin D are much, much higher (e.g., Grant et al. 2020).
Based on Blood Levels
A blood test provides a clear picture of vitamin D status. Levels are typically categorized as follows (Holick et al., 2011; Wang et al., 2017):